Table of Contents
Parametric modeling is quietly revolutionizing healthcare, offering a faster, more precise way to create custom medical devices. Imagine a scenario where a young athlete in Bangalore lost part of his leg in a road accident. His hospital referred him to a prosthetic center where he spent weeks undergoing fittings, scans, adjustments, and more fittings. The first socket didn’t fit. The second one gave him sores. The third was bearable but not ideal. It took nearly three months and a lot of frustration before he could walk without discomfort.
That’s the story for thousands of patients across the world. The problem isn’t lack of care or effort, it’s the way medical devices are designed. Most prosthetics, implants, and orthotics are still developed manually, using static templates and slow design processes that can’t keep up with the complexity of the human body.
From Templates to Tailored Healing: The Power of Parametric Modeling
In traditional workflows, prosthetics or implants are built using general measurements or adjusted manually by experienced technicians. This works in many cases, but it isn’t ideal when precision matters most. Human anatomy is unique, and even small variations can mean the difference between comfort and pain, success and failure.
Parametric modeling offers a new way to think about custom medical devices. Instead of manually redrawing each version, designers build rule-based models that adapt to different inputs like limb length, joint angle, or bone curvature. It’s not just about drawing faster. It’s about designing smarter.
The Invisible Workhorse Behind Invisalign: Parametric Modeling in Dental Tech
If you’ve ever used Invisalign or know someone who has, you’ve already seen parametric modeling in action. Invisalign takes a 3D scan of your teeth, then uses parametric algorithms to create a sequence of aligners that guide each tooth into position. A typical treatment includes 20 to 30 aligners, each slightly different from the last.
Imagine designing each of those by hand. It would be nearly impossible but with a parametric modeling workflow, the system automatically generates every stage based on the patient’s scan and treatment plan.
The result? More precision, faster turnaround, and less human error.
Custom Prosthetics That Actually Fit
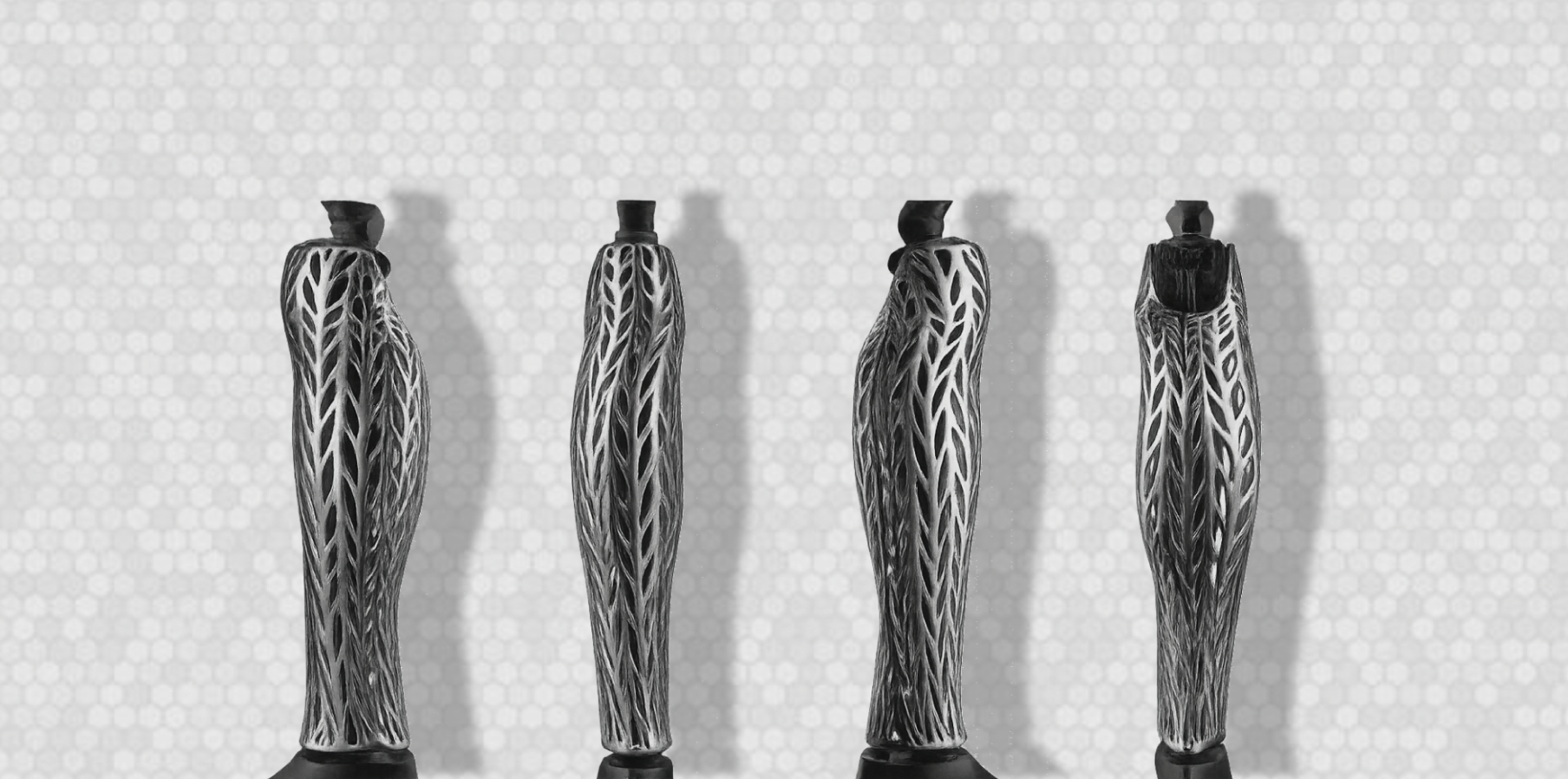
Traditional fracture casts and orthotic supports are often heavy, uncomfortable, and limit mobility but with parametric design and 3D printing, these supports can now be custom-made to perfectly fit each patient, while being lightweight and breathable.
Using a process similar to the Xkelet system described in parametric design research, the patient’s injured limb is scanned in 3D or measured precisely. This data is fed into a parametric model, which instantly adapts the structure to match the unique shape of the arm. The design optimizes both strength and ventilation, producing a modern lattice structure that supports healing while allowing the skin to breathe.
Once the model is ready, it is 3D printed in a durable, biocompatible material. The result is a custom orthosis that is strong, easy to clean, fully recyclable, and far more comfortable than traditional plaster casts. Patients can even remove it for hygiene, reducing irritation and improving their overall recovery experience.
Parametric modeling in orthotic design not only makes production faster — often within a day — but also transforms medical supports into functional, aesthetically pleasing, and patient-friendly devices.

3D Printed Lattice Arm Cast for Fracture SupportWhat used to take weeks now takes a few hours of design time and a day of printing. The difference isn’t just technical—it’s deeply human. Patients get back to walking, working, and living faster. That’s the real power of personalized design.
How BeeGraphy Makes Parametric Modeling Scalable
Platforms like BeeGraphy make parametric modeling accessible to more people. Unlike traditional CAD software that requires heavy local installs and engineering knowledge, BeeGraphy runs in the browser and lets designers build or edit parametric models without needing to write code from scratch.
For a prosthetist or biomedical engineer, this means they can collaborate with clinicians, test model variations, and generate fabrication-ready files without leaving the workspace.
Let’s say a clinic has a standard prosthetic socket model on BeeGraphy. For every new patient, they simply adjust parameters—height, stump circumference, weight class, pressure zones—and the parametric model reshapes itself in real time. No redrawing. No starting over.
And because BeeGraphy supports export to STL and DXF formats, the design can go directly to 3D printers without another software layer.
Read how parametric design works in BeeGraphy
A Typical Workflow in Medical Manufacturing
Typical workflow for custom medical devices using parametric modeling & 3D printing
-
Acquire patient data – Use a CT scan, MRI, or 3D surface scan (depending on the device). CT/MRI is common for internal implants (e.g., cranial plates, orthopedic joints), while 3D surface scans are more common for external devices like prosthetic sockets and orthoses.
-
Convert scans into 3D geometry – The scan data is processed in specialized medical imaging software (e.g., Mimics, 3D Slicer) to segment anatomy and create a clean 3D mesh.
-
Import into parametric modeling software – The segmented geometry is used as a reference or input for a parametric model (BeeGraphy could be part of this stage for certain device types, especially external prosthetics and orthotics).
-
Adjust parameters – Modify dimensions, shapes, pressure zones, and fixation points to suit patient anatomy and clinical needs.
-
Validate design – Run checks for fit, biomechanical strength, and compliance with medical regulations.
-
Export fabrication files – Save as STL, DXF, or other manufacturing-ready formats.
-
3D print with approved materials – Use medical-grade printers and certified biocompatible materials. Post-process, sterilize, and inspect before clinical use.
How Formlabs is using 3D printing for medical devices
Why 3D Printing Completes the Loop
Parametric modeling sets the rules. 3D printing makes them real.
In medical contexts, additive manufacturing is uniquely suited for custom parts. Techniques like SLA (stereolithography) and SLS (selective laser sintering) allow for high-precision parts with complex internal structures—something traditional manufacturing can’t do affordably for one-off items.
Hospitals and labs around the world are now using 3D printers to create:
- Custom surgical guides
- Dental aligners and crowns
- Orthopedic braces
- Cranial and facial implants
- Prosthetic sockets and limbs
And when those prints are based on parametric models, the production process becomes repeatable, scalable, and far more efficient.
Explore how 3D printing is reshaping healthcare – McKinsey
Why the Medical Industry Needs Parametric Modeling
In many countries, the cost of personalized medical care is still out of reach for most people. Hospitals often rely on imported parts, fixed-size templates, and slow manual design cycles. The result? Patients are left with devices that don’t fit properly, function poorly, or take months to arrive.
Parametric modeling changes this equation. By allowing designers to create adaptable, rule-based models, it enables clinics, engineers, and even small startups to deliver truly custom solutions, quickly and affordably. This isn’t innovation for innovation’s sake. It’s about solving real, human problems.
A powerful example is Team UnLimbited’s Alfie Edition, a fully parametric, 3D-printed prosthetic arm. With just a few input changes such as forearm length, wrist size, or grip type , the design can be instantly adapted for a different patient, then sent straight to a 3D printer. What once took weeks can now be done in days, bringing comfort and functionality to people who need it most.
What to Watch For
As this space grows, we’ll see more collaboration between software platforms like BeeGraphy, 3D printing labs, and healthcare institutions. But with that growth come challenges:
- Navigating regulatory approvals like FDA and CE certifications
- Ensuring biocompatible material usage
- Protecting patient data and complying with laws like HIPAA and GDPR
- Training clinicians to use parametric modeling tools effectively
None of these are dealbreakers, but they require thoughtful planning and strong partnerships between tech and healthcare.
Final Thought
The future of medicine is being shaped by smarter tools, better workflows, and more human-centered design. Whether it’s a young boy in Jaipur receiving a 3D-printed hand or an elderly man in Berlin recovering faster with a personalized hip implant, parametric modeling is changing lives quietly and effectively.
And with tools like BeeGraphy making it easier for teams to build, adapt, and manufacture, the question is no longer if this becomes standard—it’s when.